 Windsor Clinic: 0800 644 0700 -
Reading Clinic: 0800 644 0900
tannereyes@sapphire-eyecare.co.uk
Windsor Clinic: 0800 644 0700 -
Reading Clinic: 0800 644 0900
tannereyes@sapphire-eyecare.co.uk
 Windsor Clinic: 0800 644 0700 -
Reading Clinic: 0800 644 0900
tannereyes@sapphire-eyecare.co.uk
Windsor Clinic: 0800 644 0700 -
Reading Clinic: 0800 644 0900
tannereyes@sapphire-eyecare.co.uk
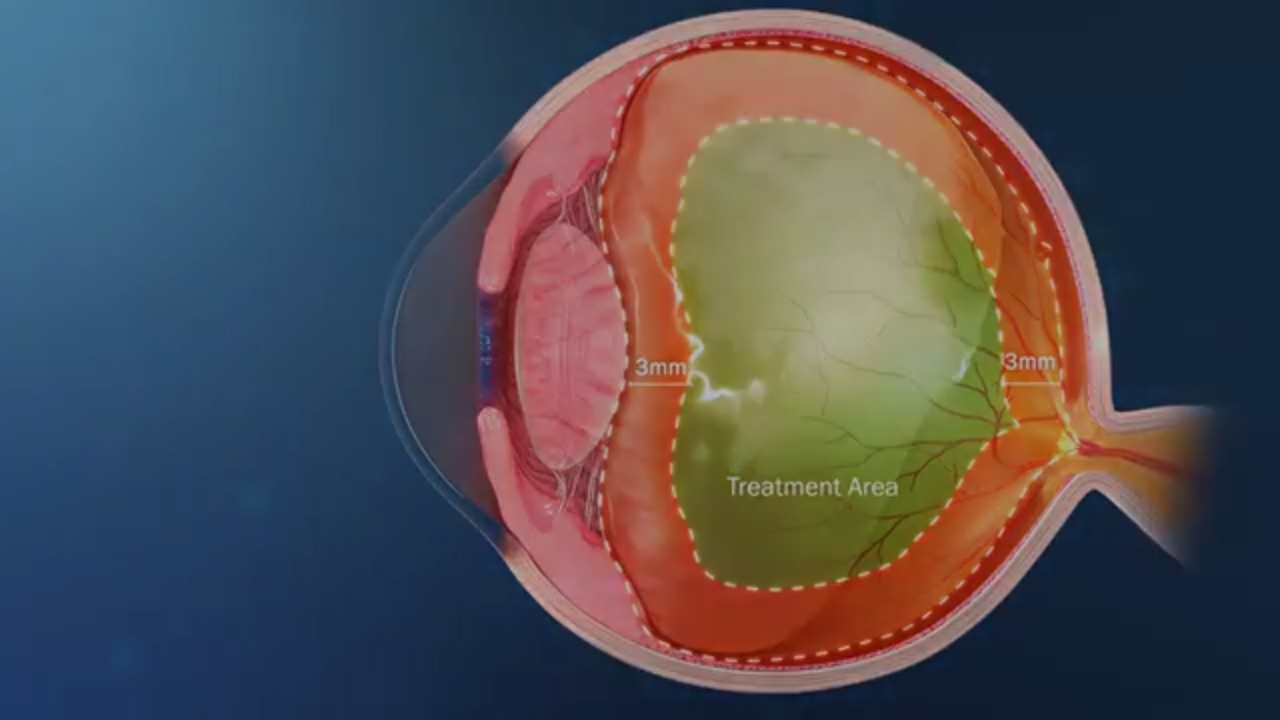
Ellex Laser Floater Treatment (LFT) Animation
Have you ever wondered what the squiggly lines that sometimes cross your vision really are? From time to time, most of us will experience these eye floaters – small specks or shapes, often like cobwebs that seem to dart away when we try to see them more clearly. People describe lines, blobs, a net curtain like effect or the “appearance of a fly” in the vision.
The appearance of floaters within the vision is usually due to age-related changes in the vitreous gel which naturally fills the eye between the lens and the retina. The gel degenerates and shrinks over time and this can cause stringy clumps of collagen fibres to form, which cast shadows on the retina. We perceive these shadows as floaters. In most patients over the age of 50 there is some visible degeneration causing clumping of the collagen fibres, which may occasionally interfere with vision.

Laser Floater Treatment
As the gel degenerates further it peels away from the retina, a process called posterior vitreous detachment (PVD). This second stage of degeneration causes additional floaters and debris together with descriptions of intermittent blur or a veil like effect in the vision. People often describe blobs, circles or a fly-like shape together with flashes of light in the vision. The flashes are due to pulling on the retina by the vitreous gel. It is this pulling which occasionally causes retinal tears and retinal detachment.
In the vast majority of patient’s eye floaters are a minor irritation with no need for treatment. However, if of sudden, recent onset then an urgent specialist examination is needed to exclude underlying serious disease which can damage vision. It is particularly important that anyone noticing sudden new floaters should be seen urgently to exclude a retinal tear which can progress to retinal detachment and sight loss. It is impossible to know just on symptoms whether a tear is present.
If the floaters are associated with a retinal tear or retinal detachment then this can usually be treated with laser or a vitrectomy surgery to prevent visual loss. However, an urgent visit to an eye doctor with a special interest in retinal disease is needed.
In the majority of patients, floater symptoms improve over a period of approximately six months but may never entirely disappear. If symptoms persist and cause problems, for example with driving or reading, then there are treatments available. Laser vitreolysis is generally considered to be safer than a surgical vitrectomy since it is less invasive. Some ophthalmologists regard eye floaters as harmless and believe that people will learn to live with them. However, there is now increasing recognition confirmed by formal scientific studies, that floaters can have a serious impact on a patient’s vision and quality of life.

Mr Tanner is not currently offering this treatment. The information below is based on preliminary studies and we await further development of the evidence base. We have left the information below as additional background for patients but vitrectomy surgery is currently the only treatment offered by Mr Tanner for removal of vitreous floater.
Also known as floater laser treatment, vitreolysis is a non-invasive, pain-free procedure that can dramatically reduce the visual disturbance caused by floaters. The goal of vitreolysis is to achieve a “functional improvement”. That is, to allow you to return to normal day-to-day activities without the interference of floaters. Laser treatment has improved significantly in recent years, with much better laser focusing allowing safer treatment. Laser is particularly effective at treating discrete, dense floaters. The types of floaters are easier to vaporise and disappear. It is very difficult to remove all floaters and debris but approximately 90% of patients report significant improvement in their vision and feel the procedure was worthwhile.
In patients with significant symptoms who are not suitable for laser treatment then vitrectomy surgery is available to remove the vitreous gel and floaters. Vitrectomy surgery is very effective at removing almost all floaters and these are some of my happiest patients. However, vitrectomy does carry significant risk and there needs to be a careful discussion prior to surgery to ensure floaters are causing a sufficient problem to justify surgery.
Vitreolysis involves the application of nanosecond pulses of laser light to vaporise the vitreous opacities and to cut vitreous strands. During this process, the floater’s collagen and hyaluronic acid molecules are converted into a gas. The end result is that the floater is either removed or reduced to a size that no longer impedes vision. Laser vitreolysis uses a Neodymium: Yttrium-Aluminum Garnet (Nd: YAG) laser to vaporise floaters within the eye.
Vitreolysis is performed as an outpatient procedure; you do not have to stay overnight in a hospital. Immediately prior to treatment, you will have anaesthetic eye drops administered. A contact lens will then be placed on your eye, with the laser light delivered through a specially designed laser microscope.
The laser is carefully aimed at either the floaters or their attachments. During treatment, you will probably see small, dark specks/shadows. These are the floaters are being vaporised into small gas bubbles. The gas bubbles quickly dissolve into the vitreous.
Each treatment session typically takes 10-30 minutes dependent on the size and extent of the floaters.
Most patients will need to undergo two treatment sessions, sometimes three, in order to achieve a satisfactory result.
Usually, it is not possible to eliminate all floaters in one sitting. The main reasons for this are:
You may observe small, dark specks in your lower field of vision immediately following treatment, which are gas bubbles and will quickly dissolve. It is also important to note that some patients may experience mild discomfort, redness or temporarily blurred vision directly following treatment.
Reported side effects and complications associated with vitreolysis are rare. Complications may include the development of cataract, retinal damage, intraocular pressure (IOP) spike and potential loss of vision (less than 1%).
Age. Patients over 45 are usually the best candidates, younger patients (<45) tend to have microscopic floaters located close to the retina. These are not considered to be good candidates for vitreolysis treatment
Onset of Symptoms. Treatment would not normally be offered to patients with less than 6 months of symptoms
Floater Characteristics. Large, well defined floaters sitting away from the retina are the best type of floater to treat with vitreolysis
Clinical studies have shown vitreolysis to be a safe, effective treatment in the majority of patients. However, if floaters persist, you may wish to consider a surgical vitrectomy. Surgery is very effective but more invasive with a higher risk of problems as described on the Vitrectomy for floaters information page
Disclaimer : The information provided in this website is intended as a useful aid to general practitioners, optometrists and patients. It is impossible to diagnose and treat patients adequately without a thorough eye examination by a qualified ophthalmologist, optometrist or your general practitioner. Hopefully the information will be of use prior to and following a consultation which it supplements and does not replace.


