
Retinal Vein Occlusion
Retinal Vein Occlusion
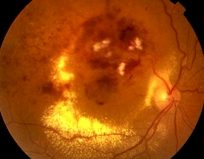
Retinal vein occlusion is a condition estimated to affect approximately 50,000 people per year in the UK. Known risk factors include high blood pressure, diabetes, high pressure in the eye and occasionally unusual blood conditions which increase the risk of clotting. The retina is the light sensitive tissue that lines the back of the eye and is responsible for the eyesight.
Vein Occlusions usually occur when a retinal vein is either:
Swelling of the macula is a secondary condition to the retinal vein occlusion. The macula is a small area in the centre of the retina that contains a rich collection of nerve cells sensitive to light, fine detail, and colour. The vein blockage causes the blood pressure to increase in the smallest vessels which causes them to bleed and leak fluid into the retina, decrease of blood flow and increase inflammation. All these processes lead to painless decrease/loss of vision in the affected eye. A similar process occurs in other inflammatory eye conditions resulting in macular swelling
Traditional treatment was laser burns to the retina which gives a small visual improvement in some cases but often does not significantly improve vision. Recently available treatments include injectable steroid (Ozurdex) and anti growth factor agents (Lucentis and Eylea)
Ozurdex contains dexamethasone which is slowly released into the eye while the implant dissolves (biodegrades). Dexamethasone belongs to a group of drugs called corticosteroids. It has been shown that it reduces inflammation, oedema, and thickening of the retina. The implant itself is very easily inserted as an outpatient procedure with minimal discomfort and rapid recovery. The drug usually lasts 4-6 months once released into the eye. The biodegradable dexamethasone implant is usually invisible to the patient and only 2mm in length.
Local anaesthetic is administered prior to the Ozurdex injection to ensure that you do not feel pain during the Ozurdex injection. The local anaesthetic is given in the form of drops or subconjunctival anaesthetic injection (under the outer covering layer on top of the white of the eye).
All injections and drugs can cause side effects in some people. Please read the section below in order to be aware of the most commonly reported side effects. Most are self-resolving or treatable with further surgery. Some will lead to visual loss. The majority of people will have significantly better vision following treatment.
Very common side effects – might affect more than one patient in 10:
Common side effects – might affect one to 10 patients in 100:
Uncommon side effects – might affect one to 10 patients in 1,000:
Some of these side effects may be caused by the injection procedure and not the Ozurdex implant itself – for example, bleeding on the surface of the eye, difficulties in seeing clearly, a feeling of spots in front of the eye (including ‘floaters’), eye pain, seeing flashes of light, swelling or scratching on the surface of the eye, a feeling of looking through mist or fog, redness of the eye, decrease in eye pressure.
Other treatment options include monthly injections of antigrowth factor agents such as Lucentis or Eylea. These drugs have also been shown to be very effective at drying macular oedema, shrinking abnormal blood vessels and improving vision. One of the main advantages of these types of injections is that they are not associated with a risk of steroid related high pressure and the injection is invisible. However, they need to be given more frequently than steroid injections (often monthly) and have a theoretically higher risk of stroke and heart attack in some individuals particularly those with uncontrolled high blood pressure or recent previous stroke.
There is a theoretical increased risk of experiencing blood clots (such as may cause heart attack or stroke) after intravitreal administration of medicines that affect the growth of blood vessels. However, a very low incidence of these events was seen in the clinical trials, similar to that seen in this age group anyway. We would normally check blood pressure before treatment. If you have had a previous stroke, please discuss this with Mr Tanner.
Risks associated with the injection process are very similar to those listed above for Ozurdex injections which you should read.
Serious complications of the intravitreal injection procedure include retinal detachment, cataract formation and infection (endophthalmitis) within the eye. Any of these serious complications may lead to severe, permanent loss of vision. In the clinical trials these complications occurred at a rate of less than 0.1% of injections.
You will receive antibiotic eye drops to help reduce the possibility of infection occurring following injection. If there are any signs of eye/eyelid infection present on the day of your planned injection, your treatment may need to be re-booked for another time to allow control of such infection. Please inform Mr Tanner or the nurse if you have a sticky or discharging eye.
Whenever a medication is used in a large number of patients, coincidental problems may occur that could have no relationship to the treatment. For example, patients with high blood pressure or smokers are already at increased risk for heart attacks and strokes. If one of these patients being treated with Lucentis/Eylea suffers a heart attack or stroke, it may be caused by the high blood pressure and or smoking and not necessarily due to eye treatment.
Your condition may not get better or may become worse despite these injections. Any or all of the complications described above may cause decreased vision and/or have a possibility of causing blindness. Additional procedures may be needed to treat these complications. During follow up visits or phone calls, you will be checked for possible side effects and the results will be discussed with you.
You can resume normal activities once you have been discharged from hospital.
I will make urgent contact if any of the following signs of infection or other complications develop: pain, blurry or decreased vision, sensitivity to light, redness of the eye (compared to immediately after the injection), or discharge from the eye. I have been instructed not to rub my eyes or swim for three days after each injection. I will keep all post-injection appointments, which may be monthly, or scheduled telephone calls so that staff can check for response to treatment and complications.
If you experience eye pain or loss of vision:
Please contact Mr Tanner’s team on 0800 644 0700 or 0800 644 0900
Out of hours Main Hospital Switchboards are:
Princess Margaret Hospital, Windsor – 01753 743434
Spire Dunedin Hospital, Reading – 01189 587676
Circle Hospital, Reading – 0118 922 6888
Eye Casualty at Royal Berkshire Hospital, Reading – 0118 322 7162/3
Disclaimer : The information provided in this website is intended as a useful aid to general practitioners, optometrists and patients. It is impossible to diagnose and treat patients adequately without a thorough eye examination by a qualified ophthalmologist, optometrist or your general practitioner. Hopefully the information will be of use prior to and following a consultation which it supplements and does not replace.


